Table of Contents
Introduction: Beyond the Hype, A New Era of Medicine
Imagine this: a patient walks into a clinic with a baffling mix of symptoms. Ten years ago, it might have taken weeks of tests and multiple specialists to arrive at a confident diagnosis. Today, an AI system can sift through millions of patient records, genomic data, and imaging scans, and within seconds, suggest likely conditions along with treatment paths. That’s not science fiction anymore, it’s the unfolding reality of AI in healthcare.
Healthcare worldwide is under strain. Populations are aging, chronic diseases are climbing, costs are ballooning, and doctors are burning out. In many countries, finding a primary care appointment has become a matter of months, not days. The system isn’t just stretched, it’s cracking. Into this stress test walks artificial intelligence, not as a silver bullet, but as a powerful collaborator.
What excites researchers and clinicians is that AI isn’t just another gadget in the medical toolbox. It has the potential to reshape the entire architecture of care. From faster artificial intelligence in medical diagnosis, to breakthroughs in AI in drug discovery, to making administrative work almost invisible, we are watching the emergence of a new medical ecosystem.
This article dives into the heart of that transformation. We’ll explore the most impactful AI applications in medicine, the real obstacles slowing adoption, and the future of AI in healthcare that is coming faster than most people expect.
The Engine Room: Key AI Applications Reshaping Healthcare Today
| Application | What it does | Examples | Impact | Timeframe |
|---|---|---|---|---|
| Precision Diagnostics | Analyzes medical images and multimodal data to detect disease earlier and more accurately. | Deep learning radiology models, pathology AI. | Earlier cancer and heart disease detection. | Now – Medium term |
| AI in drug discovery | Designs molecules, predicts protein structures, and optimizes trials. | AlphaFold, generative molecule models. | Shorter R&D, new treatments faster. | Now – Growing |
| Admin Automation | Handles notes, billing, scheduling, insurance claims. | Ambient scribes, RPA tools. | Less doctor burnout, smoother workflows. | Now |
| Personalized Medicine | Tailors therapies using genomics and patient data. | Digital twins, multi-omics AI. | More effective, fewer side effects. | Medium – Long term |
Precision Diagnostics: Seeing the Unseen
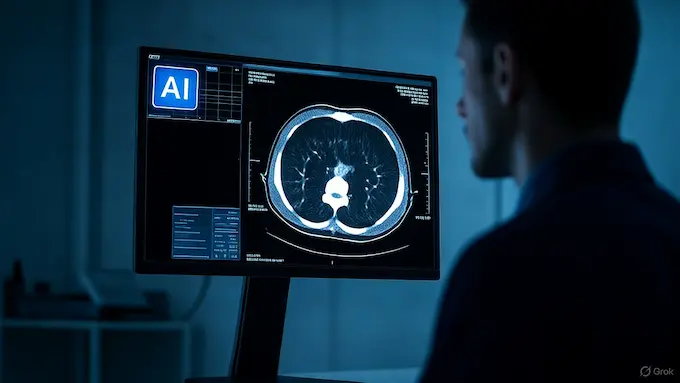
One of the most powerful promises of machine learning in healthcare is its uncanny ability to spot patterns invisible to the human eye. Radiology is the classic example. A deep learning algorithm trained on thousands of CT scans can flag a suspicious lung nodule with accuracy rivaling, and sometimes surpassing, seasoned radiologists.The human eye is a marvel, but it’s a product of evolution, not designed to find a 4-pixel anomaly in a sea of grayscale tissue. For a radiologist, the job is a high-stakes version of Where’s Waldo, played for hours on end, day after day. Fatigue is real, and the cognitive load is immense.
This is arguably the most mature application of AI in healthcare, primarily because of the massive success of deep learning, specifically Convolutional Neural Networks (CNNs), in computer vision. A CNN works in a way that’s conceptually similar to how a human visual cortex processes information. It breaks an image down into a hierarchy of features, from simple edges and textures to complex shapes and objects.
Instead of learning to spot cats or cars, we train these models on millions of annotated medical images, MRIs, CT scans, and X-rays. They learn the subtle textural differences between healthy and cancerous tissue. They learn the morphology of a tumor that suggests aggression. They learn to spot the faint shadow of pneumonia that a tired human eye might just slide over at the end of a long shift.
The results are already staggering. AI models are achieving, and in some narrow cases exceeding, human-level accuracy in detecting things like diabetic retinopathy, a leading cause of blindness, from retinal fundus images. In breast cancer screening ,AI in healthcare AI systems act as a tireless second reader, flagging suspicious mammograms for review and reducing the false negative rate. This isn’t about replacing the radiologist. It’s about giving them a collaborator that never gets tired and has perfect recall of every textbook case it’s ever seen. It’s a system for prioritizing attention, pointing to the five most concerning scans out of a hundred, allowing the human expert to focus their invaluable time and skill where it’s needed most.
Consider the workflow. A patient gets a CT scan. Before it even hits the radiologist’s worklist, an AI pre-screens it. It might identify a potential pulmonary embolism, flag it as critical, and bump it to the top of the queue. The radiologist opens the file, and the AI has already highlighted the suspicious region and even measured its dimensions. The time from scan to diagnosis is slashed, and in conditions like stroke or embolism, that time is everything.
The challenge isn’t just about accuracy. It’s about integration and trust. How do we build systems that don’t just give an answer but also show their work? The push toward “explainable AI” (XAI) is critical here. A black box that simply says “cancer” or “no cancer” is of limited use. A system that highlights the exact pixels that led to its conclusion, that presents similar cases from its database, that’s a system a clinician can collaborate with.
Take diabetic retinopathy. Left unchecked, it’s one of the leading causes of blindness worldwide. AI models can now screen retinal images at scale, picking up subtle signs of damage long before vision loss occurs. In the U.S., the FDA has already approved an AI tool that reads eye scans without requiring a specialist, opening access for rural and underserved populations.
In oncology, tools like Microsoft’s InnerEye are accelerating radiotherapy planning. What once took an oncologist hours to contour on imaging software can now be done in minutes, shaving weeks off a patient’s treatment journey. These aren’t research projects on the horizon, they are live systems making a difference today.
| AI Technology | Core Function | Primary Healthcare Application | Example |
|---|---|---|---|
| Machine Learning (ML) | Pattern recognition, prediction. | Predictive analytics, risk scoring. | Predicting sepsis risk based on vital signs. |
| Deep Learning (DL) | Hierarchical feature learning. | Medical image analysis, genomics. | Detecting tumors in CT scans. |
| Natural Language Processing (NLP) | Understanding human language. | Clinical documentation, research mining. | Transcribing doctor-patient visits into EHRs. |
| Robotics & Computer Vision | Physical task automation. | Surgical assistance, lab automation. | Guiding a surgeon’s tool for higher precision. |
AI in Drug Discovery: From a Decade to Days
Developing a new drug has traditionally been a marathon. It takes over a decade, costs billions, and has a spectacularly high failure rate. AI in drug discovery is collapsing that timeline. Algorithms are helping identify promising targets, design molecules, and predict toxicity long before costly trials.

DeepMind’s AlphaFold made headlines by predicting protein structures with stunning accuracy, cracking a challenge that had stumped biologists for 50 years. What this means is faster pathways to new therapies for conditions ranging from rare genetic diseases to widespread killers like Alzheimer’s.
Pharmaceutical giants are now partnering with AI firms to accelerate pipelines. Instead of chasing thousands of blind alleys, researchers can zero in on a handful of likely candidates. The result isn’t just faster development, it’s more precise and personalized therapeutics.
Streamlining the System: Administrative AI
If you ask doctors what they dread most, many will say paperwork. For every hour spent with patients, physicians spend nearly two on documentation and administration. That imbalance isn’t just annoying, it’s a major driver of burnout.
Enter administrative AI. Tools like Nuance’s Dragon Ambient eXperience listen to doctor-patient conversations and automatically generate structured clinical notes. Others handle billing, insurance claims, or patient scheduling with little human oversight. The impact is subtle but enormous: doctors spend more time being doctors, and patients feel less like numbers in a system.
Predictive analytics is another quiet revolution. Hospitals are using AI models to forecast emergency room surges, optimize staffing, and reduce readmissions. In complex systems like healthcare, even a 5% efficiency gain translates into massive savings and better outcomes.
Personalized and Connected Care
Perhaps the most human-facing side of AI is personalized care. Virtual assistants and chatbots, far from replacing doctors, are handling the first layer of patient interaction. Whether it’s guiding someone through symptom checks at 2 a.m. or reminding them to take medication, these systems extend care into daily life.
Wearables and ambient sensors are also becoming part of the ecosystem. An AI system can now track sleep disturbances, subtle changes in breathing, or irregular heart rhythms without the patient lifting a finger. For chronic disease management, this level of passive monitoring is a game changer.

And then there’s precision medicine. By integrating genomic data, medical history, and lifestyle factors, AI can suggest treatments tailored to the individual rather than the statistical average. The promise here is profound: medicine that doesn’t just treat populations, but respects the uniqueness of each patient.
The Human Factor: Navigating the Challenges of an AI-Augmented World
Augmenting, Not Replacing, the Clinician
Every leap in medical technology triggers a familiar fear: “Will machines replace doctors?” With AI in healthcare, the answer is clearer than ever. AI isn’t about replacing, it’s about augmenting.
AI can spot a tumor on a scan, but it can’t hold a patient’s hand during chemotherapy. It can analyze millions of health records, but it can’t weigh the emotional context of a family deciding on end-of-life care. What AI excels at is speed and scale. What humans excel at is empathy, reasoning under uncertainty, and making value-laden decisions. The sweet spot is collaboration.
The Critical Hurdles: Bias, Trust, and Accountability
For all its promise, AI applications in medicine face serious hurdles.
- Bias in data: If an AI system is trained mostly on data from one demographic group, it risks misdiagnosing patients from others. This isn’t hypothetical—it has already happened in dermatology tools less accurate on darker skin tones.
- Transparency: Many AI models are black boxes. Clinicians are rightly wary of acting on a diagnosis they can’t interrogate. Explainable AI is a growing field, but progress is uneven.
- Liability: If an AI tool recommends a treatment that harms a patient, who’s accountable? The developer? The hospital? The clinician? Legal systems are only beginning to wrestle with these questions.
The Road to Adoption: Integration and Regulation
Even the best AI model is useless if it doesn’t fit into real clinical workflows. Electronic health records are notoriously clunky, and plugging AI into them isn’t trivial. Then there’s the regulatory landscape. Bodies like the FDA are creating frameworks for approving AI medical devices, but the pace of innovation often outruns policy.
Trust, workflow integration, and regulation will determine whether AI becomes a universal tool or remains a patchwork of pilot projects.
The Horizon: The Future of AI in Medicine
By 2030, the market for AI in healthcare is projected to reach nearly $187 billion. That’s not just hype it’s a reflection of how central AI is becoming across every corner of medicine.
In the near term, expect more adoption of AI-powered diagnostics and virtual assistants. In the medium term, machine learning in healthcare will mature to integrate multimodal data: imaging, genomics, wearables, and clinical notes all feeding into unified models. That’s when digital twins virtual replicas of patients will move from concept to practice. Doctors could simulate treatments on your digital twin before ever prescribing in real life.
In the long run, the future of AI in medicine points toward anticipatory care. Instead of waiting for symptoms, AI could predict disease years in advance, offering interventions that prevent illness altogether. Combine this with breakthroughs in AI in drug discovery, and medicine shifts from reactive to proactive, from population averages to hyper-personalized care.
| Country / Region | Initiatives / Players | Primary Fields | Adoption Level | Notes |
|---|---|---|---|---|
| United States | Tech giants, startups, academic centers. | Diagnostics, drug discovery, telehealth, analytics. | High | Strong private sector investment, broad deployments. |
| United Kingdom | NHS pilots, health-tech startups, academia. | Imaging, monitoring, national screening. | High | Government-led programs, regulatory focus. |
| India | Telemedicine platforms, screening startups. | Cancer, eye disease screening, rural telehealth. | Medium | Expanding access in underserved regions. |
| China | AI firms, hospitals, government programs. | Imaging, triage, genomics, population health. | High | Strong central investment, rapid hospital rollout. |
| Germany | Health-tech pilots, clinical collaborations. | Documentation, radiology, data platforms. | Medium | Focus on privacy, interoperability. |
Conclusion: A Call for Responsible Innovation
The promise of AI in healthcare isn’t just faster diagnoses or cheaper drugs. It’s the chance to redesign healthcare into something more equitable, efficient, and humane. But technology alone won’t get us there.
The real determinant will be how we use it. Do we embed fairness into algorithms? Do we ensure access extends beyond wealthy hospitals to rural clinics? Do we design AI to free doctors for deeper human connection instead of drowning them in new digital tasks?
If medical imaging is about pattern recognition, drug discovery is about navigating an impossibly vast search space. The traditional path to a new drug is a brutal marathon of trial and error that can take over a decade and cost billions of dollars. We screen tens of thousands of chemical compounds hoping to find one that interacts with a specific biological target, like a protein involved in a disease, in just the right way. Most of them fail.
AI in healthcare is turning this needle-in-a-haystack problem into a guided search. It’s compressing the timeline at multiple stages of the pipeline.
1. Identifying Targets: First, you need to know what to aim for. AI models, particularly those using Natural Language Processing (NLP), can ingest and synthesize the entire corpus of biomedical research, patents, and clinical trial data. They can connect the dots between genes, proteins, and diseases in ways no human research team could, identifying novel biological targets that are more likely to be effective.
If we do it right, the partnership of human expertise and machine intelligence can deliver a future of medicine that is not only smarter but kinder.
1. How is AI used for medical diagnosis and treatment?
AI is widely used to analyze medical images, detect early signs of diseases like cancer or diabetic retinopathy, and suggest treatment options. It supports clinicians by providing pattern recognition and predictive insights that complement human expertise.
2. Will AI in healthcare replace doctors and clinicians?
No. AI augments doctors rather than replaces them. It handles repetitive, data-heavy tasks, allowing clinicians to focus on empathy, critical thinking, and complex decision-making.
3. What are the biggest challenges and risks of using AI in medicine?
The main challenges are biased training data, lack of transparency in model decisions, integration with clinical workflows, and unresolved legal questions about liability.
4. Can artificial intelligence help reduce overall healthcare costs?
Yes. By cutting diagnostic delays, optimizing hospital operations, and accelerating drug discovery, AI has the potential to reduce costs across the system while improving outcomes.
5. How does AI technology improve the patient experience?
AI enables faster diagnoses, personalized treatment plans, continuous health monitoring via wearables, and easier access to care through virtual assistants, all of which improve patient experience and engagement.